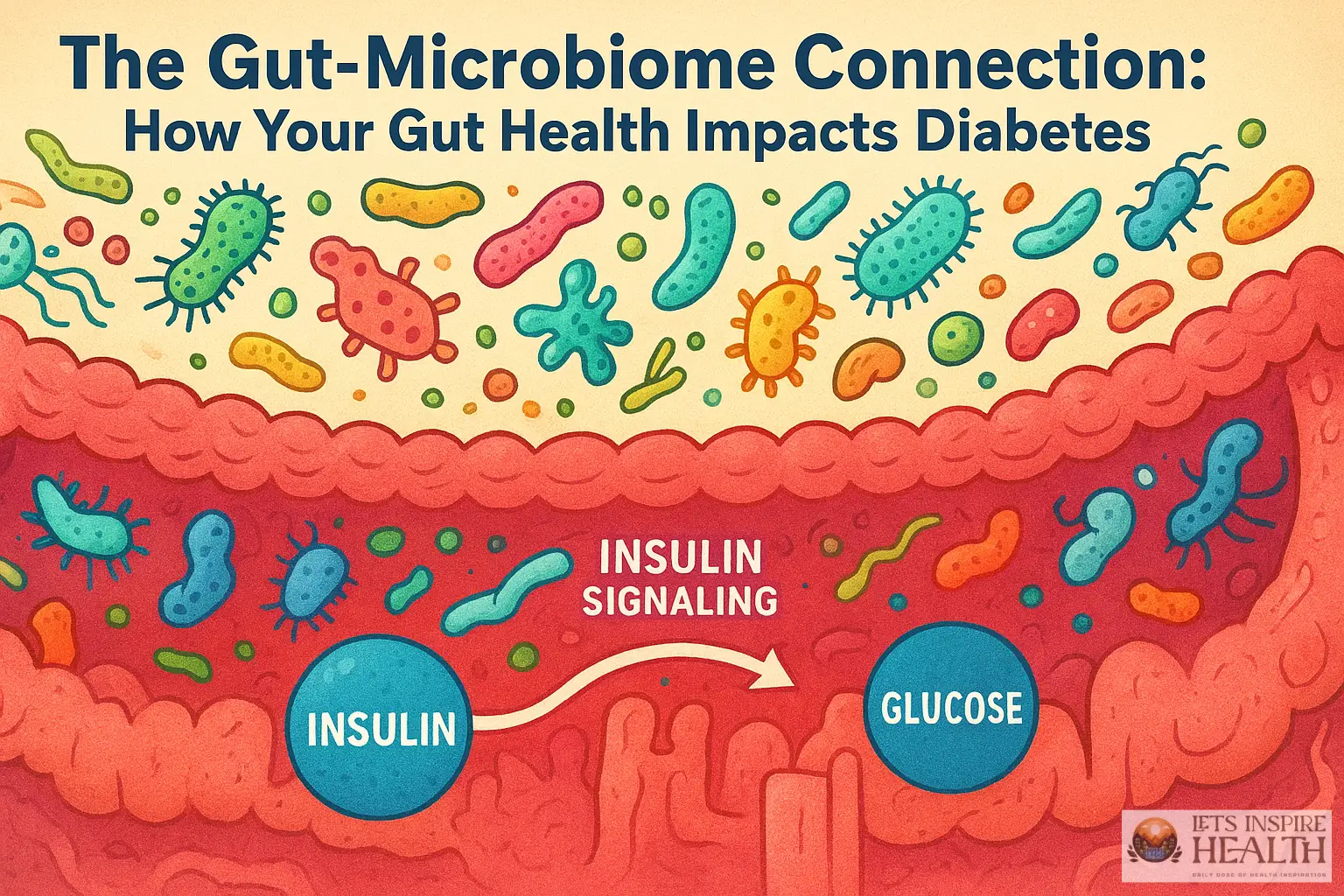
Have you ever wondered if the key to managing your diabetes wasn’t just about medication and diet, but something far more intricate – the health of your gut? The gut microbiome, the trillions of bacteria and other microorganisms living in your digestive system, is increasingly recognized as a powerful player in the development and progression of type 2 diabetes. It’s a fascinating and complex relationship, and understanding it could revolutionize your approach to managing this chronic condition. Let’s delve into the gut-microbiome connection and how nurturing your gut health can significantly impact your diabetes journey.
Understanding the Gut Microbiome
The gut microbiome isn’t just a passive resident; it’s a bustling ecosystem with profound effects on your overall health. These microorganisms perform a myriad of functions, including digesting food, synthesizing vitamins (like K and B vitamins), training the immune system, and even influencing brain function through the gut-brain axis. The composition of your microbiome – the types and amounts of bacteria present – is influenced by a variety of factors, including your genetics, diet, lifestyle, and medication use.
Dysbiosis, an imbalance in the gut microbiome, is frequently observed in individuals with type 2 diabetes. This imbalance can lead to impaired glucose metabolism, insulin resistance, and inflammation – all key contributors to the disease. Studies have shown that people with diabetes often have a reduced diversity of bacterial species compared to healthy individuals. This lack of diversity can weaken the gut’s ability to effectively regulate blood sugar levels.
Pros of Understanding the Microbiome: Increased awareness of the role of gut health in diabetes management. Potential for personalized interventions based on individual microbiome profiles. Cons: Complexity of the microbiome makes it difficult to pinpoint specific causes and solutions. Potential for over-interpretation of microbiome data.
How the Microbiome Impacts Insulin Resistance
Insulin resistance, where cells become less responsive to insulin’s signal to take up glucose from the bloodstream, is a central feature of type 2 diabetes. Emerging research suggests that the gut microbiome plays a significant role in driving this resistance. Certain bacterial species can produce metabolites – byproducts of their metabolism – that directly interfere with insulin signaling pathways.
For example, short-chain fatty acids (SCFAs), primarily acetate, propionate, and butyrate, are produced when gut bacteria ferment dietary fiber. Butyrate, in particular, has been shown to improve insulin sensitivity by enhancing mitochondrial function – the powerhouses of our cells – and reducing inflammation. Conversely, an overabundance of certain bacteria can produce lipopolysaccharides (LPS), a potent inflammatory molecule, which contributes to insulin resistance.
Effects on Human Health: SCFAs can improve glucose control and reduce inflammation. LPS can exacerbate insulin resistance and contribute to chronic inflammation. Step-by-Step Tutorial: To increase butyrate production, focus on consuming a high-fiber diet rich in foods like bananas, berries, and leafy greens.
Diet and the Microbiome – A Powerful Combination
Your diet is arguably the single most influential factor shaping your gut microbiome. A diet high in processed foods, refined sugars, and saturated fats can promote the growth of harmful bacteria and reduce microbial diversity, while a diet rich in fiber, fruits, and vegetables supports a healthy and diverse microbiome.
Key Dietary Strategies:
- Increase Fiber Intake: Aim for at least 25-35 grams of fiber per day.
- Fermented Foods: Incorporate fermented foods like yogurt (with live cultures), kefir, sauerkraut, kimchi, and kombucha into your diet. These foods contain probiotics – live beneficial bacteria – that can directly populate your gut.
- Prebiotic Foods: Prebiotics are non-digestible fibers that feed beneficial bacteria. Excellent sources include garlic, onions, leeks, asparagus, and oats.
Effects on Human Health: Increased microbial diversity leads to better metabolic health. Probiotics can improve gut barrier function and reduce inflammation. Real-World Example: A study published in *Diabetes Care* demonstrated that individuals with type 2 diabetes who consumed a high-fiber diet experienced significant improvements in HbA1c levels – a key marker of long-term blood sugar control.
Probiotics and Prebiotics – Targeted Interventions
While dietary changes are crucial, supplementing with probiotics and prebiotics can provide a targeted boost to your gut health. However, it’s important to note that not all probiotics are created equal. The effectiveness of a probiotic depends on the specific strains used, as different strains have different effects.
Probiotic Strains of Interest for Diabetes: *Lactobacillus* and *Bifidobacterium* species have shown promise in improving insulin sensitivity and reducing blood sugar levels in some studies. Research is ongoing to identify the most effective strains for individuals with type 2 diabetes.
Prebiotic Supplementation: Inulin, fructool, and resistant starch are common prebiotic supplements that can nourish beneficial bacteria.
Effects on Human Health: Probiotics can modulate the immune system and improve gut barrier function. Prebiotics enhance the growth of beneficial bacteria, leading to increased SCFA production. Caution: Some individuals may experience temporary digestive discomfort (gas, bloating) when starting probiotic supplementation. Start with a low dose and gradually increase it as tolerated.
Monitoring Your Gut Health – Tools and Techniques
Understanding your gut health is an ongoing process. There are several tools and techniques you can use to monitor your microbiome and assess its impact on your diabetes management.
- Stool Testing: Fecal tests can analyze the composition of your gut microbiome, providing valuable insights into bacterial diversity and abundance.
- Breath Testing: Some breath tests measure the levels of specific volatile organic compounds (VOCs) produced by gut bacteria, offering a non-invasive way to assess microbiome activity.
- Dietary Tracking: Keeping a detailed food diary can help you identify dietary patterns that are positively or negatively impacting your gut health.
Effects on Human Health: Regular monitoring allows for personalized interventions. Early detection of dysbiosis can enable timely adjustments to diet and lifestyle. Important Note: Consult with a healthcare professional before starting any new supplement or dietary regimen.
Summary
The gut-microbiome connection is increasingly recognized as a critical factor in the development and management of type 2 diabetes. By understanding the complex interplay between your gut bacteria and your body, you can make informed dietary and lifestyle choices that support a healthy microbiome, improve insulin sensitivity, and ultimately, better control your blood sugar levels. This journey requires a holistic approach, combining dietary modifications, targeted supplementation (when appropriate), and regular monitoring to achieve optimal gut health and diabetes management.
Disclaimer: This blog post is for informational purposes only and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. The information presented here should not be used as a substitute for professional medical advice. We are not responsible for any adverse outcomes resulting from the use of this information. Diabetes management requires personalized care and ongoing monitoring by a healthcare provider. This blog post does not endorse any specific products or supplements.