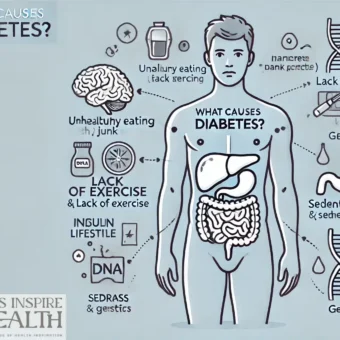
Living with diabetes can feel like navigating a complex landscape – a constant balancing act between medication, diet, and lifestyle. While conventional treatments are undeniably crucial, many individuals are increasingly exploring complementary therapies to manage their blood sugar levels, improve overall well-being, and enhance their quality of life. This exploration delves into the world of complementary therapies for diabetes management, examining the potential benefits, drawbacks, and how they can be integrated into a holistic approach. We’ll look at options ranging from mindfulness and acupuncture to dietary supplements and traditional practices, providing a balanced perspective to help you make informed decisions about your health journey.
Mindfulness and Meditation for Diabetes Management
The mind-body connection is a powerful one, and chronic stress significantly impacts blood sugar levels. Mindfulness and meditation practices can help regulate the nervous system, reduce stress, and improve insulin sensitivity. Studies have shown that regular meditation can lower HbA1c levels – a key marker of long-term blood sugar control. The process itself involves focusing on the present moment, observing thoughts and feelings without judgment. This doesn’t require hours of sitting; even 10-15 minutes a day can make a difference.
How it Works: Stress triggers the release of cortisol, which can elevate blood sugar. Mindfulness helps counteract this by activating the parasympathetic nervous system (the “rest and digest” response), promoting relaxation and reducing cortisol levels.
Step-by-Step Tutorial:
- Find a Quiet Space: Choose a place where you won’t be disturbed.
- Get Comfortable: Sit in a chair with your feet flat on the floor, or sit cross-legged on a cushion.
- Focus on Your Breath: Close your eyes and pay attention to the sensation of your breath entering and leaving your body.
- Acknowledge Distractions: When your mind wanders (and it will!), gently bring your attention back to your breath.
- Start Small: Begin with 5-10 minutes and gradually increase the duration as you become more comfortable.
Pros: Non-invasive, readily accessible, can be practiced anywhere, improves emotional well-being.
Cons: Requires consistent practice, may not be effective for everyone, can be challenging to maintain focus.
Acupuncture for Diabetes: Balancing Energy Flow
Acupuncture, a traditional Chinese medicine technique, involves inserting thin needles into specific points on the body to stimulate energy flow, or “Qi.” Research suggests acupuncture can improve insulin sensitivity, lower blood sugar levels, and reduce complications associated with diabetes. The theory behind it is that imbalances in Qi can contribute to physiological dysfunction, including those seen in diabetes.
How it Works: Acupuncture is believed to influence the nervous system, releasing endorphins – natural pain relievers and mood boosters – and potentially affecting the autonomic nervous system, which controls blood sugar regulation.
Research Findings: Several studies have indicated that acupuncture can be as effective as conventional treatments for managing diabetes, particularly in terms of HbA1c reduction.
Important Note: Always seek a qualified and licensed acupuncturist experienced in treating diabetes.
Pros: Can significantly lower blood sugar, reduces pain and discomfort, has minimal side effects.
Cons: Can be expensive, some individuals may experience mild discomfort during treatment, requires multiple sessions.
Dietary Supplements for Diabetes Management
Certain dietary supplements can play a supportive role in managing diabetes, but it’s crucial to approach them with caution and under the guidance of a healthcare professional. Some supplements that have shown promise include chromium, magnesium, alpha-lipoic acid, and berberine. These supplements are often taken to improve insulin sensitivity, enhance glucose metabolism, and protect against oxidative stress.
Chromium: A trace mineral that may improve insulin sensitivity and glucose control.
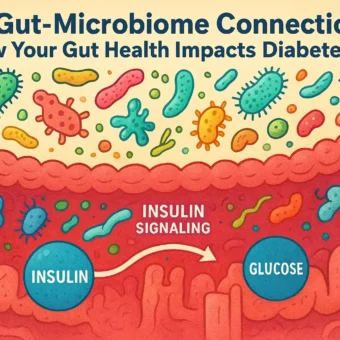
Magnesium: Plays a role in insulin signaling and glucose metabolism.
Alpha-Lipoic Acid (ALA): An antioxidant that can protect against oxidative stress and improve insulin sensitivity.
Berberine: A plant alkaloid that has shown promise in lowering blood sugar levels and improving insulin sensitivity.
Important Disclaimer: Supplements can interact with medications. Always inform your doctor about any supplements you are taking.
Pros: Can be taken alongside medication, potentially enhances the effectiveness of conventional treatments.
Cons: Can be expensive, potential for interactions with medications, quality control can vary.
Traditional Practices: Yoga and Tai Chi
Yoga and Tai Chi are mind-body practices that combine physical postures, breathing techniques, and meditation. Both can improve insulin sensitivity, reduce stress, and enhance overall well-being. The gentle movements and focus on breath can positively impact the nervous system, promoting relaxation and reducing the physiological effects of stress.
Yoga: Focuses on holding poses (asanas) while coordinating breath and movement. Certain styles, like Hatha yoga, are particularly suitable for beginners.
Tai Chi: Characterized by slow, flowing movements that promote balance, coordination, and relaxation. It’s a low-impact exercise that can be beneficial for individuals with diabetes.
Research Support: Studies have shown that Tai Chi can significantly improve glycemic control in individuals with type 2 diabetes.
Pros: Improves flexibility, balance, and coordination, reduces stress, enhances mindfulness.
Cons: Requires learning proper techniques, may not be suitable for everyone with physical limitations.
Integrating Complementary Therapies: A Holistic Approach
It’s essential to remember that complementary therapies are best viewed as supportive additions to conventional diabetes management. They should not replace prescribed medications or lifestyle recommendations. A holistic approach combines conventional treatments with complementary therapies, focusing on overall well-being – physical, mental, and emotional. Working closely with your healthcare team – including your endocrinologist, primary care physician, and a qualified complementary therapy practitioner – is crucial for developing a personalized plan that addresses your individual needs and goals.
Key Considerations:
- Communication: Keep your healthcare team informed about any complementary therapies you are using.
- Monitoring: Regularly monitor your blood sugar levels and other health indicators.
- Realistic Expectations: Understand that complementary therapies may not provide a “cure” for diabetes but can contribute to improved management and quality of life.
Disclaimer: This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. Self-treating can be dangerous. This blog post is not a substitute for professional medical advice.